The earliest evidence of humanity’s understanding of heart disease is found in ancient Egypt, Greece, and Mesopotamia. Studies on ancient Egyptian mummies have shown that heart disease was commonplace. There is also an ancient Egyptian relief that depicts a human with a bird cage to the left of the center of their chest, exactly where the heart is. Some archaeologists argue that the bird in the cage represents irregular heartbeats, a common symptom of Atrial Fibrillation.
Sir William Harvey Was The First To Scientifically Confirm atrial fibrillation
The English physician and physiologist, Sir William Harvey (1578-1657), was among the first to take a more modern scientific approach towards heart disease. His best known work, Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus (Latin for “An anatomical exercise on the movement of the heart and blood in living beings”), published in 1628, describes the close connection between heartbeat, heart rate, and blood circulation.
Harvey stated that “there is only one cause of the heartbeat in the body (which is felt at the wrist or on the neck (my addition)) and that is the contraction of the left ventricle”. He also argued that the pulse in the pulmonary circuit (the small circuit) is due to the contraction of the right ventricle.
Through observations on dying animals Harvey was also able to observe that the last structure in the heart that ceased contracting on death was the right atrium, more specifically the right atrial appendage, or auricle. He also noted that just prior to death heart contractions became irregular and rapid.
Harvey’s work demonstrated that:
- The heart acts as a muscle pump that is responsible for the blood circulation in the body (“the large circuit”) and through the lungs (“the small circuit”).
- The heart rhythm is controlled from the right atrium, more specifically from an area around the origin of the auricle of the right atrium. This is the exact location of what we now call the “sinus node”, which regulates our heartbeat.
- The heart rhythm may – in certain circumstances – be irregular. As the noted irregularity was in the right atrium, Harvey’s text can be considered the first “correct” description of atrial fibrillation (AF).
Knowledge and information spread much more slowly during the renaissance. It would be more than 100 years before Harvey’s ingenious observations were taken up and further developed. In the intervening period the prevailing view was that the heart and arteries operated independently, due to observations that heartbeats and the observable pulse did not always correspond.
Jean-Baptiste de Sénac Built On These Observations
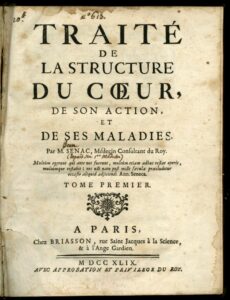
It wasn’t until 1749, with the publication of Jean-Baptiste de Sénac’s (1693-1770) work Traité de la structure du coeur, de son action et de ses maladies, that atrial fibrillation would be directly referenced. The work confirmed Harvey’s observation of atrial fibrillation in the dying heart, and also that normal heartbeats originate from the upper right atrium, where we now know that the sinus node is located.
Additionally de Sénac observed that strain on the heart could have an impact on the contraction of the heart. This was based on observations of patients with “febris rheumatica” (Rheumatic fever), where an infection of the throat with common streptococcus bacteria could cause a secondary inflammatory condition of the heart valves.
In 1909, the English physician and researcher, Dr. Thomas Lewis, referenced “auricular fibrillation” (another word for atrial fibrillation still found in French medical parlance as “fibrillation auriculaire”) in a short article: “Auricular Fibrillation: A Common Clinical Condition” published in “The British Medical Journal”.
Thomas Lewis Recorded Some Of The Earliest Atrial Fibrillation Treatments
Thomas Lewis described atrial fibrillation as a very frequent companion to narrowed mitral valve – again with by studying the, at that time, common disease rheumatic fever. He described the common symptoms of AF in more detail than previous publications.
Specifically he noted the completely irregular and rapid electrical discharge from the atria of the heart and the varying conduction of these impulses to the ventricles of the heart, with the consequent varying pulse rate. He also noted that this electrical “flicker” in the atria affected more than just the pulse rate. It could also impact the strength of the pulse. When the heart beats quickly, the pulse rate would be weaker – when it beat slower, the pulse beats became stronger. Longer gaps between heartbeats would allow the left ventricle to fill with more blood, pumping more blood through the body.
This discrepancy between the heart rhythm and the measurable pulse had previously been understood that the heart and arteries operated independently of each other. Lewis was the first to confirm that in reality the pulse rate simply reflected the amount of blood entering the left ventricle, and therefore the volume of blood pumped around the body.
Natural medicines
Additionally Lewis was among the first to understand why digoxin, extracted from the digitalis plant, slows the pulse when a patient has atrial fibrillation. He explained that this worked by breaking the impulse line through the AV-node, the relay station between the atria and the heart chambers. Interestingly the first types of medicine that had a confirmed effect against atrial fibrillation are natural medicines, specifically quinine and digitalis.

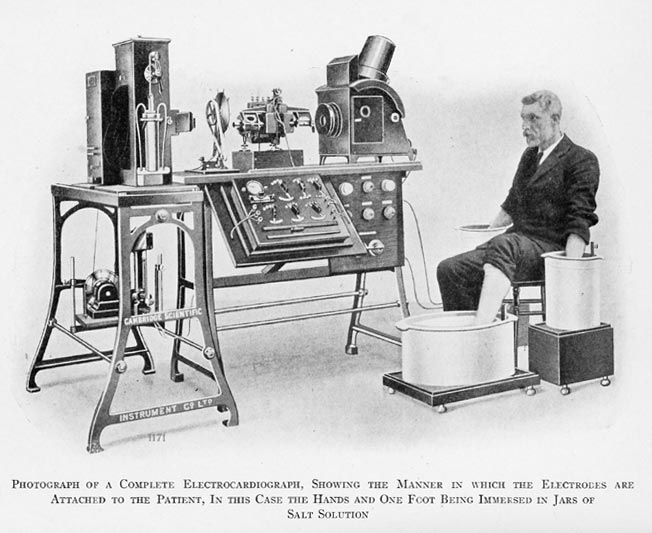
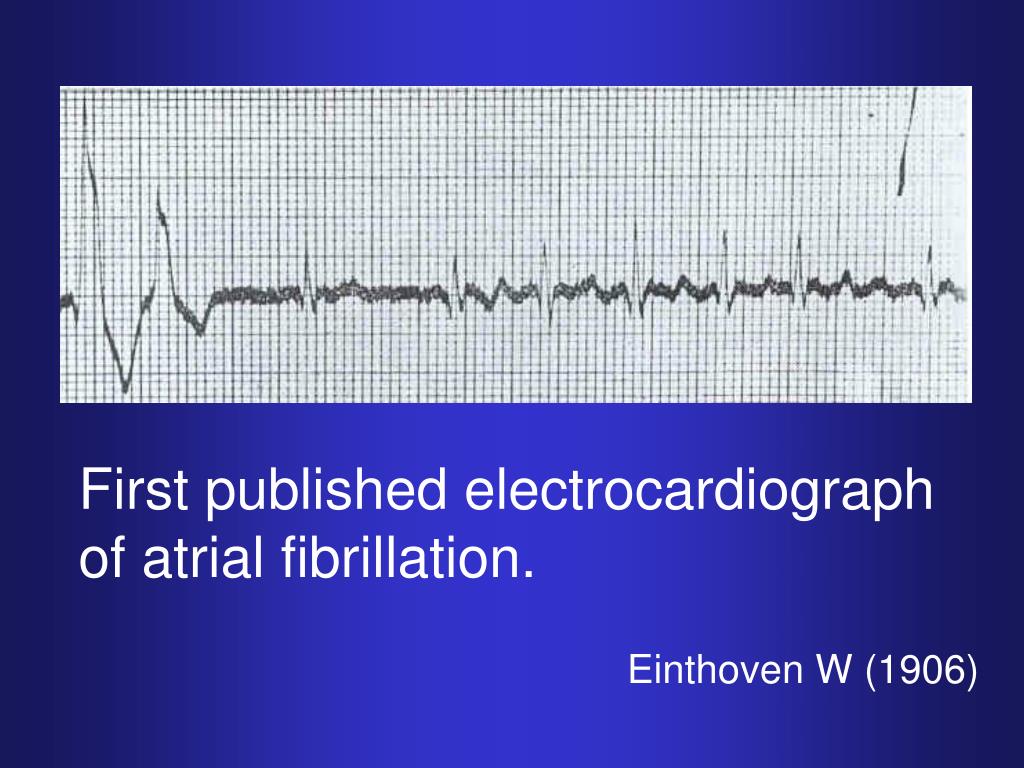
Lewis’ observations were based partly on simultaneous measurements of heart rate curves and observations of the heart’s contractions and partly on “ECG recordings” of the heart’s electrical activity. ECG recordings had recently become possible on the basis of equipment developed by the Dutch physician and researcher Willem Eindthoven in the years 1901-1903.
Thomas Lewis also made another observation, which later became important for the treatment of atrial fibrillation. He showed that he could provoke atrial fibrillation in animal hearts by dripping a certain chemical substance on the “auricle” of the left atrium. If he then divided the auricle into smaller and smaller pieces, he reached a point where it was no longer possible to provoke the fibrillation. He thus demonstrated that a certain amount of cohesive heart muscle tissue is needed in order to make it fibrillation.
George Ralph Mines hypothesis
This knowledge, together with the English researcher George Ralph Mines’ discovery (1909) that the electrical impulses in the heart can form circles, led the American physiologist GR Moe to formulate a hypothesis that atrial fibrillation is conditioned by a number of circular waves which are established in the atria and which can change in number as well as anatomical localization over time.
Sinus rhythm
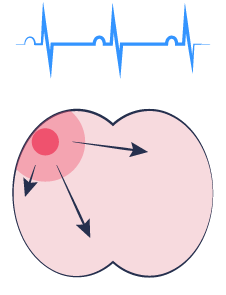
Coordinated activity over atria
Atrial fibrillation
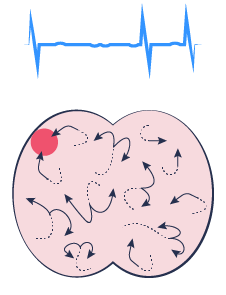
Migrating waves of re-entrant activation
This explains the chaotic electrical activity from the atria that can be observed on an ECG recording during atrial fibrillation. And it also explains the observation that the initiation of atrial fibrillation is always preceded by one or more “extra beats” (“extrasystoles”), which are known to be able to start “circus movement disorders” (also known as “re-entry tachycardia”) in the heart rhythm.
James Cox Developed The First Cardiac Surgical Technique To Treat Atrial Fibrillation
The American heart surgeon, James Cox, was also interested in atrial fibrillation – a heart rhythm disorder that is often seen in the aftermath of heart surgery. He decided to take a thorough look at the scientific literature – even far back in time, a thoroughness that is unfortunately often neglected in modern medical science.
Cox was inspired by “circular disorders” together with Lewis’ finding that there must be a certain critically coherent mass of heart muscle tissue for the fibrillation to occur and be maintained. He used this knowledge to develop a cardiac surgical technique to treat atrial fibrillation.
The operation consists of making surgical incisions in the right and left atria and subsequently sewing them back together. This separates smaller areas of the atrial muscles from scar tissue which act as barriers to electrical impulse conduction.
At the same time, the surgical incisions helped to connect structures in the heart, which also constitute barriers to electrical impulse conduction. This is to reduce the risk of “circus movement disturbances” of the heart rhythmaround the lines of scar tissue.
The treatment also needed to ensure that there was a continued electrical connection between the structure in the right atrium that triggers our heartbeat (the “sinus node”) and the structure through which the impulses are conducted from the atria to the heart chambers (the “AV node”). To do this the impulses were thus to be conducted through a maze of smaller pieces of heart muscle from the “sinus node” to the “AV node”. This operation came to be known as the Cox Maze procedure.
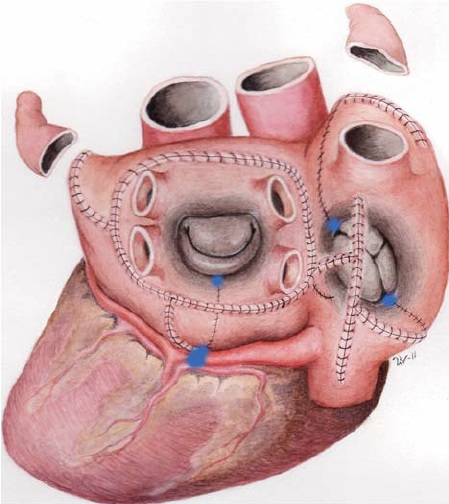
The operation was refined over several iterations until the final version was found – Cox ‘Maze III procedure. Since then, the operation has been further developed with the use of cold ablation (“cryoablation”) as an alternative to cutting through the muscles with a scalpel. This is called the Cox Maze IV procedure.
This Knowledge Formed The Basis of Modern Atrial Fibrillation Treatments
The knowledge gained about “circus movements rhythm disorders” and electrical impulses in the heart has formed the basis of the development of drugs to treat atrial fibrillation. These substances are used for rhythm control, a treatment strategy that aims to prevent AF from occurring, and stop it if it starts.
The majority of these drugs were developed in the 1960s, 1970s and 1980s. Well known examples include amiodarone / Cordarone 1961, flecainide / Tambocor 1985, and sotalol / Sotacor 1964/1974. The most recent development is Multaq / dronedaron, which came on the market in 2009.
Knowledge that the impulse conduction through the AV node can be medically inhibited has led to the use of “beta blockers” (eg metoprolol, atenolol, bisoprolol), “calcium blockers” (eg verapamil, diltiazem) and “digoxin”, which all – among others – have this effect.
This knowledge also led to the first treatment using catheter based ablation. The aim here is to destroy the AV Node or the bundle of His so that impulses can no longer be conducted from the atria to the ventricles of the heart. The first AV-node or bundle of His ablations were performed using powerful electric shocks in the heart, aimed at the AV-node or the bundle of His. This was called “Fulguration” and was first described by the American cardiologists Scheinman and Gallagher in 1982 and 1983, respectively.
From around 1990, physicians began to use the much more gentle “radio frequency ablation”, where you send a kind of microwave into the tissue and thus heat the muscle tissue sufficiently to be destroyed locally. Radiofrequency ablation continues to be used extensively, and has proven to be both effective, controllable and gentle.
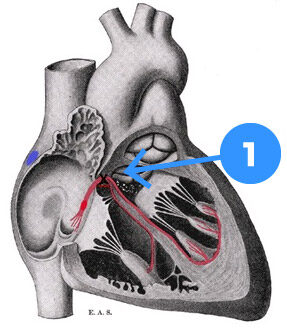
- Bundle of His
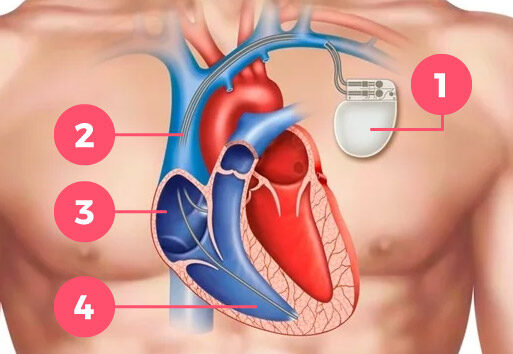
- Pacemaker
- Pacemaker-leads
- Right atrium
- Right ventricle
If you disconnect the impulse line from the atria to the heart chambers, there is no longer anything to regulate the heart rhythm – and thus the pulse. It is therefore necessary to implant a pacemaker, which must provide a sufficient number of impulses to the heart, both at rest and during activity.
In the 1990s a team led by Professor Michel Haïssaguerre improved the ablation procedure
In the mid-1990s, a group of cardiologists from Bordeaux, led by Professor Michel Haïssaguerre, documented that “extrasystoles” (additional heartbeats that occur outside the physiological heart rhythm) are needed to start episodes of atrial fibrillation. These extrasystoles generally originate from close to where the blood vessels from the lungs enters the left atrium with oxygenated blood to the body. Scientists still do not fully understand why these areas are particularly prone to generate extrasystoles.
It is possible that these areas are particularly prone to tension and pressure when the heart is stressed. And this pulling and pressing effect then causes the heart muscle cells in these areas to fire electrical impulses (extrasystoles).
Ablation for atrial fibrillation
Haïssaguerre and his colleagues also demonstrated that one can perform an electrical isolation of these areas via radiofrequency ablation through small instruments (called “catheters”) that can be inserted into the heart through the blood vessels. This knowledge has become the basis of how to perform ablation for atrial fibrillation today.
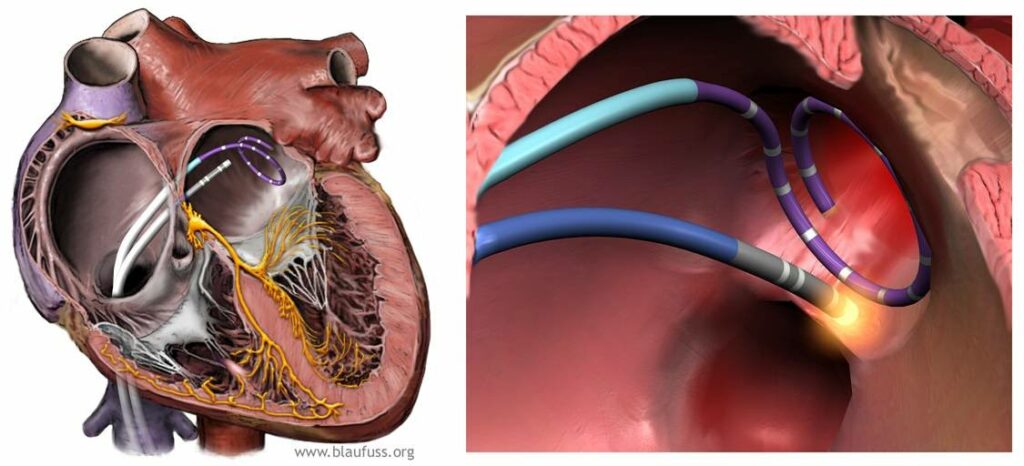
Ablation (heat treatment / burning) around the openings of the pulmonary veins into the left atrium
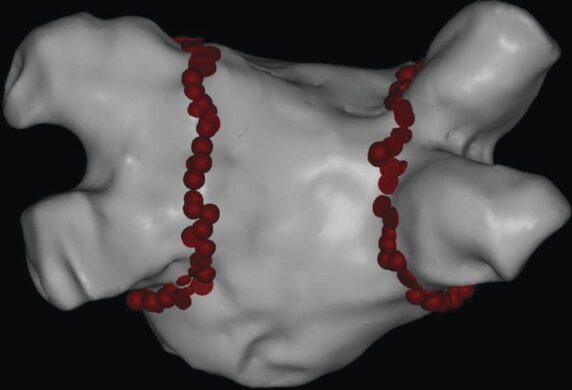
Marking on a 3-dimensional mapping during ablation treatment of the places that have been heated / burned.
Ablation treatment has spread all over the world, and there are hundreds of thousands of ablations performed to treat atrial fibrillation every year. Both our increased understanding of how to most effectively perform ablation treatment and the technological development over the past 20 years means that it is possible to remove atrial fibrillation in up to 90% of patients who suffer from periodic atrial fibrillation, known as paroxystic atrial fibrillation.
Dr. Moe’s theory of multiple / many circular disorders may not 100% explain the occurrence of atrial fibrillation. Additionally, extrasystoles from the areas around the pulmonary veins probably can not 100% explain all episodes of atrial fibrillation either.
There is still much research work underway to give us even more knowledge about why atrial fibrillation occurs and how it can best be treated. It will be especially beneficial to gather better knowledge about how we best treat patients with persistent atrial fibrillation. Where the results of ablation treatment today are inferior to those in patients with periodic atrial fibrillation.