Atrial fibrillation is by far the most common heart rhythm disorder. About 3% of the population has atrial fibrillation, and about one in four (25%) can expect to get atrial fibrillation during their lifetime.
Atrial fibrillation may occur periodically (called “paroxysmal atrial fibrillation”) or may be present constantly (called “persistent” or “permanent” atrial fibrillation). Often, atrial fibrillation will initially be periodic, but gradually become more and more frequently and tend to last longer on average. And after a while – months to years – there will be a tendency for atrial fibrillation to develop to be present all the time. Unless you do something to get rid of it. Solutions include medical treatment, electrical conversion or ablation.
Sinus rhythm
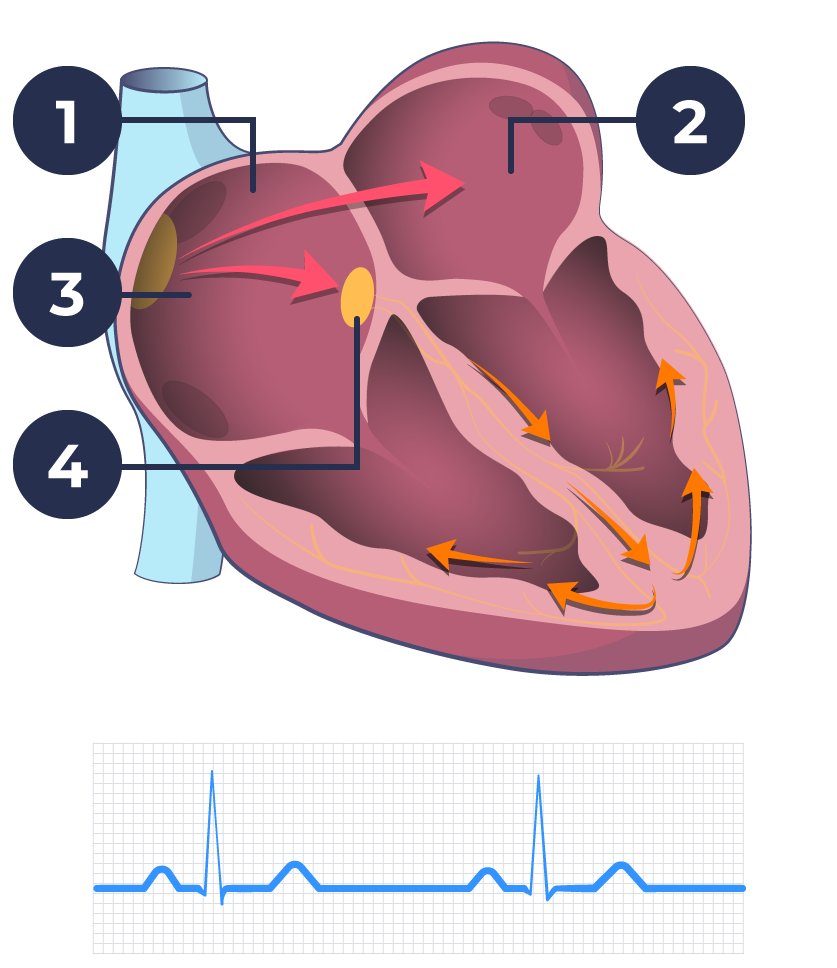
Atrial fibrillation
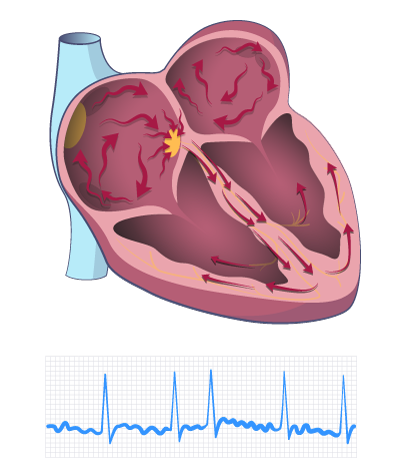
When you have atrial fibrillation, the electrical activity in the atria of the heart (“atria”) is very fast. This results in 300-500 pulses per minute. This can mean that the atria do not drain properly of blood for each heartbeat. It also means that the pulse becomes completely irregular.
When the atria fails to properly drain blood, it might begin to clot – just as it does when you get a cut. If you are unlucky a blood clot can break away and flow from the heart and out into the rest of the body, unfortunately often into the brain. This can cause a stroke.
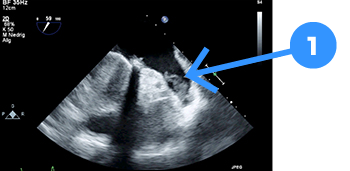
- Blood clot in the auricle of the left atrium
Atrial fibrillation may be present without you even noticing it. This is when the condition is most dangerous as you are at a heightened risk of a blood clot, even though you do not know it. This is why it is important for you to understand the most common symptoms of atrial fibrillation:
- An Increased tendency to lose breath, especially with physical activity
- Reduced physical capacity
- Increased tendency to fatigue
- More frequent urination
- Inability to concentrate
- Restless heartbeat
Atrial fibrillation typically does not cause chest pain. You may experience occasional dizziness or a feeling of having to faint, but this is not typical. The most common symptoms – shortness of breath, reduced physical capacity and increased tendency to fatigue – are caused by the heart being unable to efficiently pump oxygen, and therefore energy, around your body.
Diagnosis and treatment
There are three important goals for diagnosis and treatment:
- Ensure that the patient has the best quality of life possible
- Reduce the risk of blood clots
- Reduce strain on the heart
First, of course, your doctor must confirm that atrial fibrillation is present. This is very simple in the case of constant atrial fibrillation. You just have to take an electrocardiogram – a so-called ECG. This can be done by the family doctor and you can immediately determine if there is atrial fibrillation.
The situation is more complicated in the case of periodic atrial fibrillation. Like periodic errors in the computer or in the car, it can also be challenging to “catch” atrial fibrillation that occurs periodically. One way to do so is to learn how to feel your own pulse. I have previously written about this here.
Irregular pulse may be a sign of atrial fibrillation
If your pulse occasionally feels irregular, it may be atrial fibrillation. In this case you should talk to your doctor about it. Doctor’s are able to make a long-term recording of your heart rhythm. This process is called Holter monitoring or R-test or Event ECG. These are registrations where you get a small device with electrodes mounted on your chest. The device can then record your heart rate over several days. In rare cases, a small recorder can be implanted under the skin. This can last for up to three years and is programmed to “capture” episodes of atrial fibrillation.
It can be difficult to distinguish between frequent extra beats (“extrasystoles”) and atrial fibrillation when using traditional methods, such as taking your pulse.
Fortunately, there are new technologies on the way that will make it much easier to determine if episodes of atrial fibrillation occur.
Technology and apps to help track atrial fibrillation
For example, it is possible to use various “Apps” on smartphones to measure the heart rate at your fingertips. However, it can still be difficult to distinguish between extra beats and a afib. To help assist you, there are various solutions on the way in the market. These new solutions can immediately record a real ECG when you feel something “wrong”. And then very easily forward the recording to your cardiologist. This kind of technology (for example Apple Watch 4, or later generations or AliveCor) will gain a lot of ground within the next few years.
If you suspect you may have atrial fibrillation, you should see a professional to examine the heart for any errors. This examination is undertaken by a cardiologist, often using a technique called echocardiography. This is an ultrasound examination of the heart, where you can assess the heart’s function, heart valves, emptying force, etc. In this way, you can examine whether there is a defect in the heart – for example, a leaky heart valve – which has caused strain and thus atrial fibrillation. Or whether the afib has affected the ability of the heart to pump blood, leaving excess blood in your heart chambers. At the same time, a blood test will also be examined for measures of metabolism, diabetes and kidney function.
Anticoagulants
Based on these tests, your doctor can then assess whether it would be advisable for you to start taking blood-thinning medication. This type of medication reduces the risk of blood clots very significantly. However, not everyone with atrial fibrillation should be advised of blood thinners. It depends on a number of factors including: age, high blood pressure, diabetes, other heart disease, reduced emptying power etc.
Physicians can not simply recommend blood-thinning medication to anyone with atrial fibrillation – or to anyone where atrial fibrillation is suspected. This is because blood-thinning medication may increase your risk of bleeding. The drug works by inhibiting clotting factors in the blood, rather than by thinning it. This increases the risk of a patient experiencing dangerous levels of bleeding, which means that a physician needs to ensure that the prescription will do more good than harm. See my previous post about this.
What happens next?
Based on an overall assessment of your symptoms, the impact on your heart and the assessed risk of blood clot complications, your physician- together with you – will be able to make a sensible plan for treatment and follow-up.
It is important to recognize that atrial fibrillation is most often a chronic disorder. This means that there will be conditions that must be considered over time. You may not have any discomfort at present, but may develop more discomfort as you get older, or have longer periods of afib. You may have a very low risk of blood clot complications now, but you get a greater risk the older you get. Or if you get high blood pressure or diabetes later in life.
A treatment that works well for you now is not necessarily the best treatment in two or five years. In addition to giving you an understanding of what atrial fibrillation is, what it does to you and what can be done to reduce symptoms and risk, I therefore always recommend that you make a follow-up plan. It may be with the family doctor, but often it will also be a good idea to see a cardiologist from time to time.