The most serious complication of atrial fibrillation is a blood clot, specifically a blood clot in the brain. Approximetly 25% of all strokes due to blood clots are due to atrial fibrillation. Around 900,000 Americans annually suffer from a blood clot in the brain, where approximately 120.000 of them are caused by atrial fibrillation.
- Blood clots in the brain are the most serious complication of atrial fibrillation.
- Not everyone needs to have blood-thinning medication.
- Assessment of blood clot risk is called CHADS-VASc.
- Assessment of bleeding risk is called HAS-BLED.
- If blood-thinning medication is not tolerated, the left atrial appendage can be closed.
Risk of Blood clots With Atrial Fibrillation
Unfortunately atrial fibrillation increases the risk of blood clots, as during an episode the atria is not able to properly drain, meaning that there may be blood left in the heart that is not circulated around the body, which eventually clots. A blood clot may “tear itself loose” – a bit like when a glacier breaks an iceberg – and is carried out into the body with the blood flow from the heart. Unfortunately most often to the brain.
The positive news is that many of these incidents can be prevented using anticoagulants, also known as blood-thinning medication. This type of medicine reduces the blood’s ability to clot. However, not everyone should be advised to take blood thinners. It depends on the risk of blood clots in the atrial fibrillation.
Your physician can make a statistical assessment of the risk of blood clots by including various factors in an overall assessment using a model called the “CHADS-VASC score”:
The presence of each factor counts one point – however, an age higher than 75 years counts for two points and previous blood clots in the brain also counts for two points. You can thus get a maximum of 9 points. One point can be translated into an annual risk of a blood clot complication for atrial fibrillation of 1.3% and 9 points to an annual risk of 15.2%. Female gender alone is not counted if no other risk factors are present. If you have two points or more, it will usually be advisable to take blood-thinning medication.
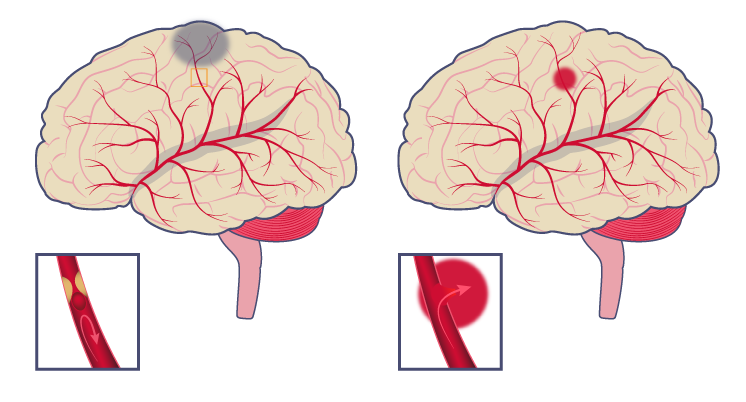
| Blood clot |
| A blocked blood vessel prevents the blood from reaching certain areas |
| Bleeding |
| A rupture of a blood vessel causes the blood to leak into the brain |
The downside of anticoagulants is that reduced clotting ability may increase the risk of bleeding. The colloquial term blood-thinner leads to a misunderstanding about how anticoagulants work. The blood does not specifically get thinner, instead its ability to clot is reduced. This increases the risks of bleeding, and can make otherwise innocuous injuries dangerous.
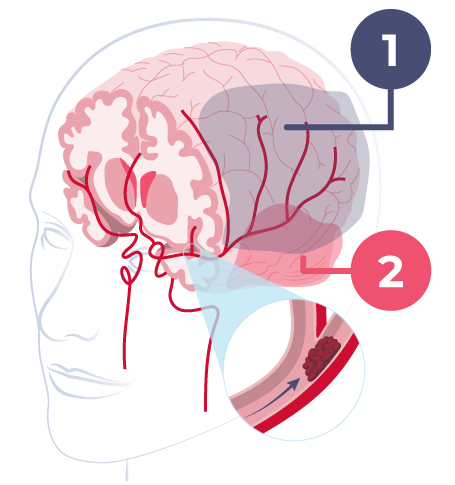
- Penumbra
- Core
This is why it’s important for a physician to ensure that there is a net gain to the patient for taking blood-thinning medication. To do this there is a statistical tool to assess a patient’s risk for excessive bleeding called HAS-BLED, which is also rated on a score of 9:
Several of the risk factors are the same as those in the CHADS-VASC score (High blood pressure (Hypertension), age, previous strokes etc.). This means that a common factor such as “high blood pressure” can be both a risk factor for blood clots and for bleeding.
If you compare the relationship between score and bleeding frequency (= bleeding rate) or blood clot risk, there are two factors that are important. The first is that the increase in bleeding risk with higher scores, is not as sharp as it is for the risk of blood clots. The second, the highest bleeding rate is not as high as the blood clot risk.
This means that with a CHADS-VASC score of 2 or more, there must be significantly more risk factors for bleeding before the net benefit of anticoagulants is overcome by the risk of the bleeding.
Blood-thinning medication
Many people, including doctors, are apprehensive about prescribing blood-thinning medication to elderly patients due to the presumed risk of falls, which comes with a higher risk of internal bleeding. However, all things considered, the risk of a blood clot in the brain generally outweighs the risk of prescribing anticoagulants.
A few years ago I heard a very fine lecture from a distinguished elderly and retired British professor of heart disease. He had made the effort to try to figure out how many times an elderly person with atrial fibrillation would have to fall for the overall risk of more severe bleeding to exceed the beneficial effect of blood-thinning medications in preventing blood clots. More than 370 falls a year – or more than one fall a day – were needed before the gain was offset by the risk of bleeding. And after all, there are few elderly people who have such frequent episodes of falls …….
Closing the left atrial appendage closure can help prevent blood clots
Usually one will give blood-thinning medication such as, Eliquis (apixaban), Xarelto (rivaroxaban), Pradaxa (dabigatran), Lixiana (edoxaban) or Warfarin, to prevent blood clots. However, some patients may not tolerate these types of medications or have a preexisting condition with a high risk of bleeding. It is also possible that anticoagulants do not work for all patients.
In that case, it is possible to close the left atrial appendage, where most blood clots form. There are various ways to do this. The most common treatment is to insert a form of membrane, which then closes the blood flow both to and from the left atrium. It is a very simple operation that can be performed through the vascular system from the groin. You can read more about the operation here.
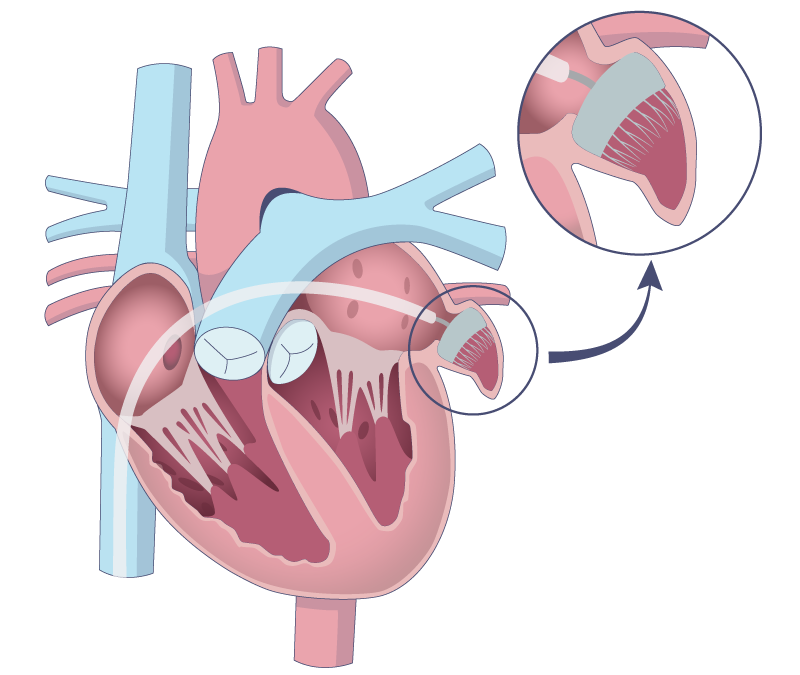
The above illustration demonstrates how the heart ear can be closed. A physician locates the closing area using ultrasound scanning, called TEE. A few weeks to months after the membrane has been placed, heart cells will cover the membrane and the patient can stop taking anticoagulants.