One of the most serious complications of atrial fibrillation is a blood clot in the brain. These clots originate from the left atrium of the heart, and most often in a structure within the left atrium, which is called the auricle. This is because atrial fibrillation patients are unable to effectively drain the blood from the left atrium to the left ventricle. As the blood isn’t drained it can clot, and this clot can travel to the brain. This leaves atrial fibrillation patients with two options: Take anticoagulant medication, or undergo an auricular closure procedure.
Most Physicians Will Prefer To Try Anticoagulants First
Doctors will usually opt to provide blood thinning medication, such as Eliquis (apixaban), Xarelto (rivaroxaban), Pradaxa (dabigatran), Lixiana (edoxaban) or vitamin K antagonists (e.g. Warfarin). However, not all patients can tolerate these kinds of medications, or they may cause more harm than good by increasing the risk of a cerebral hemorrhage.
In these cases it is possible for physicians to perform closure of the left atrial auricle. There are various ways to do this, but the most common use is to insert a form of membrane into the heart. This eventually closes the blood flow both to and from the left atrial appendage. It is a simple operation that can be performed through the vascular system from the groin.
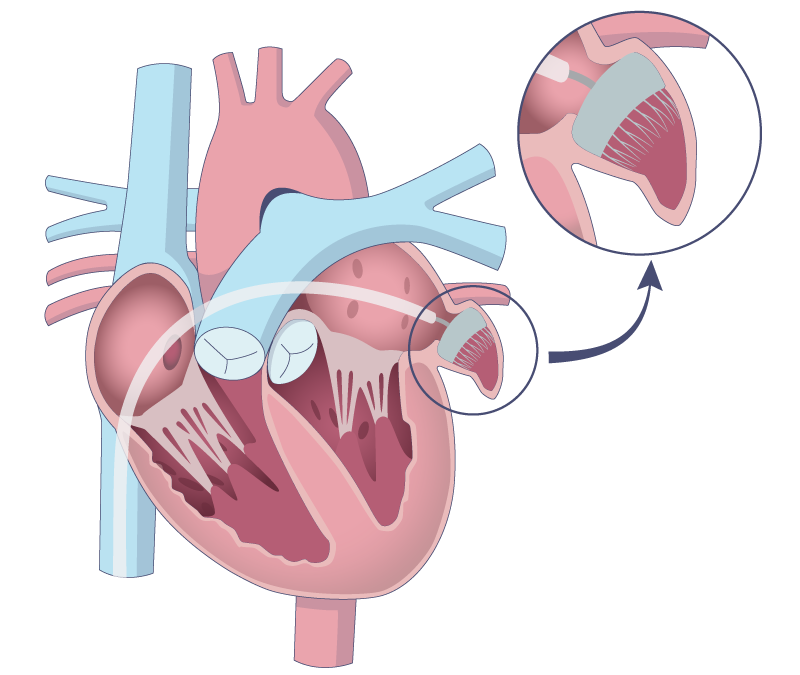
The above illustration demonstrates how the left atrial appendage can be closed. The location of the closing mechanism is ensured during simultaneous ultrasound scanning from the esophagus (so-called TEE) or from inside the heart (so-called ICE). After a few weeks to months, the closure mechanism is covered by heart cells growing over the membrane. At this point you can then stop taking blood-thinning medication.