The most serious complication of atrial fibrillation is a blood clot in the brain, and anticoagulants are one of the best ways to avoid this. These medications, often called blood thinners, prevent your blood from clotting, which is a big problem for sufferers of atrial fibrillation.
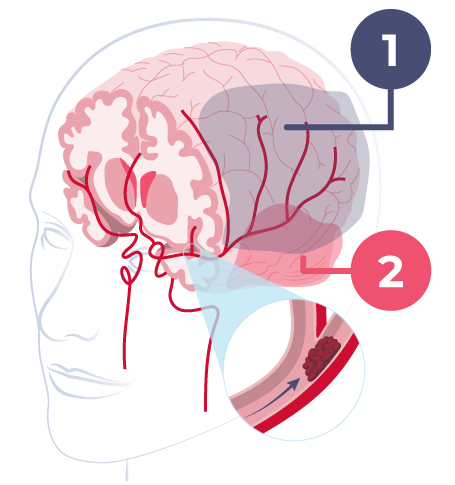
- Penumbra
- Core
Blood Clots Are Hugely Dangerous
Blood clots can form in a variety of organs, such as the heart, kidneys, intestines, and brains. These blood clots typically originate in the left atrium. This is because patients with AF struggle to drain the blood from the left atrium to the left ventricle, which means that pools of blood form.
This blood eventually begins to clot, and if this clot detaches from the left atrium it will use your blood vessels to enter other parts of your body. This means that the blood often ends up in the brain, where it can settle as a clot. The problem is so acute that 25% of all blood clots in the brain are due to atrial fibrillation.
The implications of a blood clot can vary wildly. However, they typically include paralysis, impaired speech and vision, memory, and in the worst case even death.
Anticoagulants Can Counter This
The risk of blood clots in atrial fibrillation can be reduced very significantly if you are treated with so-called blood-thinning medication. It is a type of medicine that reduces the clotting ability of the blood. The downside of this approach is that reduced clotting ability may increase the risk of excessive bleeding.
This means that physicians need to be careful when weighing the pros and cons of blood thinners. To do this, they have developed a model known as the CHA2DS2-VASc score. This model takes a variety of factors and uses them to create a score out of 9 points for each patient:
| Condition | Points | |
| C | Congestive heart failure (or Left ventricular systolic dysfunction) | 1 |
| H | Hypertension: blood pressure consistently above 140/90 mmHg (or treated hypertension on medication) | 1 |
| A2 | Age ≥75 years | 2 |
| D | Diabetes Mellitus | 1 |
| S2 | Prior Stroke or TIA or thromboembolism | 2 |
| V | Vascular disease (e.g. peripheral artery disease, myocardial infarction, aortic plaque) | 1 |
| A | Age 65–74 years | 1 |
| Sc | Sex category (1 point if male) | 1 |
One point can be translated into an annual risk of a blood clot complication for atrial fibrillation of 1.3% and 9 points to an annual risk of 15.2%. Female gender alone does not count if no other risk factors are present.
Example Case: a 70-year-old woman with atrial fibrillation, high blood pressure, and diabetes.
She would have a CHA2DS2-VASc score of 1.5 (age) + 1 (female) + 1 (high blood pressure) + 1 (diabetes 2), or a total of 4.5. This can be translated into an annual risk of a blood clot (most likely in the brain) of about 6%. Equivalent to one in 16.
How Do Blood Thinners Work?
There are various types of blood thinners available. The common feature of all of them is that they inhibit the formation of certain clotting factors in our liver by blocking vitamin K.
Vitamin K is a necessity for the formation of some of these clotting factors. Most of the medicines used as anticoagulants are designed to counteract the effect of vitamin K. The most widely used of these drugs is Marevan.
Doctors measure this effect with regular blood tests and a measurement called INR. A patient should have an INR rate of between 2 and 3. If the number is too low then more medicine is needed, if it is too high then the dose needs to be reduced. There are many factors that can affect this level, including foods high in vitamin K, such as cabbage and certain other vegetables, or alcohol.
Within the last decade, new types of blood-thinning medications have entered the market. The most well known are Xarelto, Pradaxa, Lixiana and Eliquis. These protect just as well against blood clots as Meraven but they reduce the risk of a cerebral hemorrhage in comparison. These medications must be taken as a fixed dose, and are not affected by food or drink.
Many doctors will prefer one of the four new drugs when starting blood thinning treatment. However, patients must continue with marevan if you have had a heart valve changed to a “mechanical” heart valve.
If you are being treated with Marevan and have not experienced any side effects, you do not need to change.