Atrial fibrillation (AF) is the most commonly diagnosed form of arrhythmia. One in four of us will be diagnosed with AF at some point in our lives. Around 3% of the Danish Today, approximately 1,5 mill UK citizens and up to 6 mill US citizens suffers from AF.
Atrial fibrillation falls into two categories:
- Paroxystic atrial fibrillation – The patient experiences the symptoms of AF episodically with normal heart rhythm (“sinus rhythm”) in between
- Persistent or Permanent atrial fibrillation – The patient experiences the symptoms of AF constantly without intermittent periods of normal heart rhythm
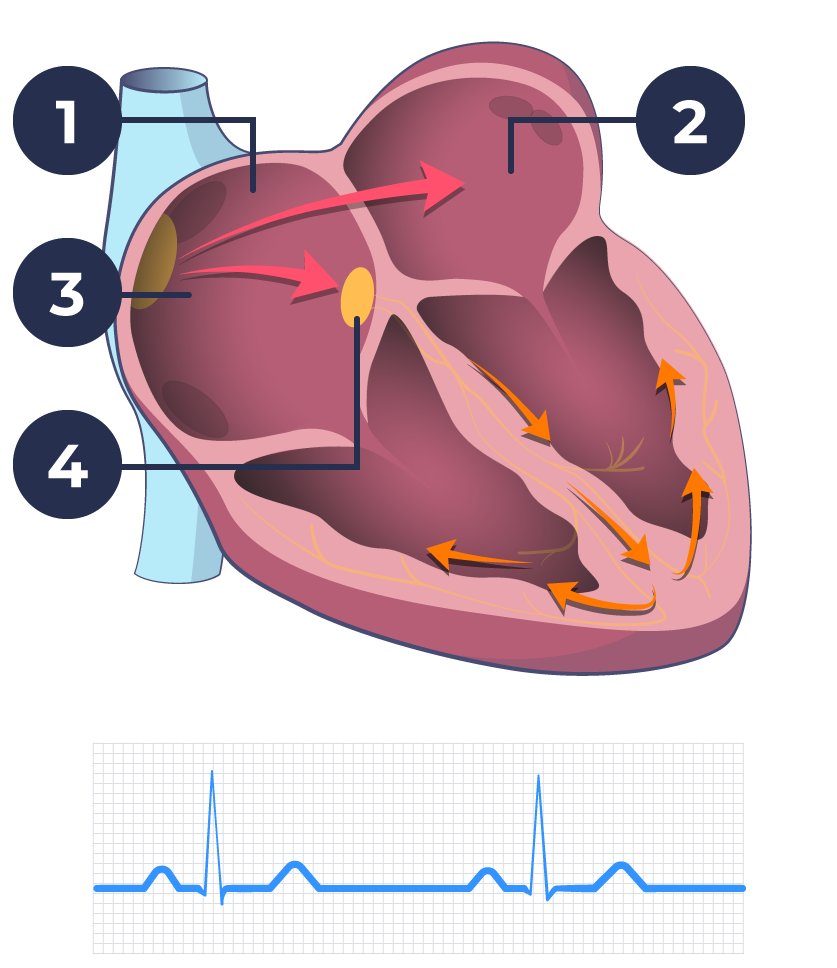
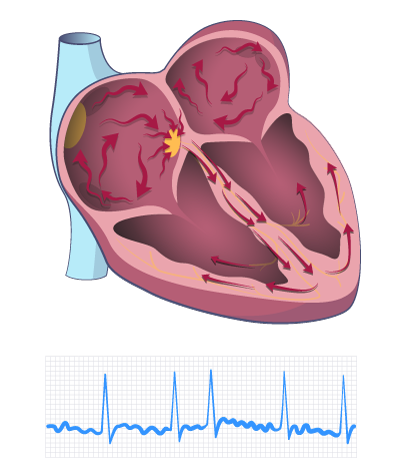
When a patient has atrial fibrillation it means that the mechanisms that regulate heart rate are not functioning correctly. Instead of receiving regular impulses from the sinus node (known as sinus rhythm), there is a chaotic series of impulses in the atria of the heart. This problem can send as much as 600 stimuli per minute to the AV node, which is only capable of conducting up to approximately 200 stimuli per minute.
This overload of stimuli lead to a patient’s pulse becoming completely irregular. The pulse will often become significantly faster than it would normally be. Fortunately, the AV node only allows a limited number of impulses to be transmitted from the atria to the ventricles of the heart. If this wasn’t the case, you would probably die the very first time you experienced atrial fibrillation.
Sinus rhythm
Atrial fibrillation
During an episode of atrial fibrillation, the heart will be unable to pump blood efficiently. This means that the body receives less oxygen and, therefore, less energy than usual. This can lead to a number of symptoms, including:
- You feel short of breath more often
- You become tired more easily than normal
- You notice a restless heartbeat
- You need to urinate more regularly during the onset of AF
- You often lose concentration
Factors to consider when deciding how to treat Atrial Fibrillation (AF)
There are three main factors to consider when deciding how to treat AF:
- Atrial fibrillation may increase the risk of developing precursors to blood clots in the left atrium. These can be carried with the blood flow to the brain and settle as blood clots, thereby giving rise to a stroke. In order to avoid this, your doctor may recommend that you start a course of treatment using blood-thinning medications.
- Is your heart rate generally within the acceptable range, or is it running faster than it should be? Over time a rapid pulse can affect the ability of the heart to pump blood. This may lead to heart failure.
- How much are you bothered by your atrial fibrillation? The impact of your symptoms on your daily life will be a major factor in determining the level of treatment you require.
Treatment for atrial fibrillation strives to reduce the risk of blood clots and to give you the best possible quality of life. When deciding on the best course of treatment for atrial fibrillation, there are two main strategies:
- To accept the presence of atrial fibrillation, but ensure that the impulse transmission from the atria to the ventricles does not become too fast. This is called “frequency control”
- Try to directly treat and eliminate atrial fibrillation, either with medication or with an ablation. This is called “rhythm control”
Recent studies on treatment of Atrial Fibrillation (AF)
Recent studies indicate that “rhythm control” reduces the risk of cardiovascular death and the risk of stroke, compared to “frequency control” – with equal numbers of patients treated with blood thinning medications among the two groups of patients. The same holds true for patients with heart failure, who may expect survival benefits by “rhythm control”. This, together, probably will turn medical practice into a more active “rhythm control” strategy.
4 comments